A two-month-old baby has saved his life upon being implanted with a splint in the trachea in a hospital in Michigan (USA), which was reproduced in a 3D printer, as published today in The New England Journal of Medicine.
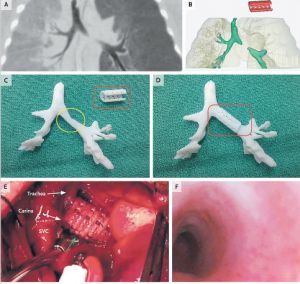
The newborn suffered constant attacks caused by a syndrom called tracheobronchomalacia, which prevents oxygen from reaching the lungs due to a problem in the trachea problem, as diagnosed by doctors who have published the study. In view of the situation, doctors decided to print a kind of splint, which reproduced the tracheal tube based on a tomographic image of the child's airway.
The 3D reproduction is made with a material called polycaprolactone, bioabsorbable by the human body in three years, so the patient doesn't need another surgery to have the implant removed. The implant was reproduced on the printer in less than a day.
According to doctors, when the implant is removed naturally, the child's lungs and airways will be developed enough to stay open by themselves. After inserting the tube, doctors kept the baby on life support for 21 days, after which the baby was allowed to leave the hospital. One year after implantation, there have been no rejection or any problem with breathing.
This case demonstrates, doctors conclude in the study, that the combination of high resolution images plus the computer design and biomaterials for 3D printing can facilitate the creation of precise anatomical implants. The study has been signed by Scott Hollister and Richard Ohye from the University of Michigan, and Marc Nelson from Akron Children's Hospital.
The three-dimensional printers are making headway in medicine, but for now the applications are very limited. Initially, they were used to design conventional solid materials intended to design personalised implant prosthesis. One of the benefits is the ability to create custom models at lower prices than conventional industrial processes. The next step, as the case published today in the New England Journal of Medicine, is to design objects with a biological material such as the biodegradable polymer employed in the intervention to reproduce the trachea fragment that the patient was missing.
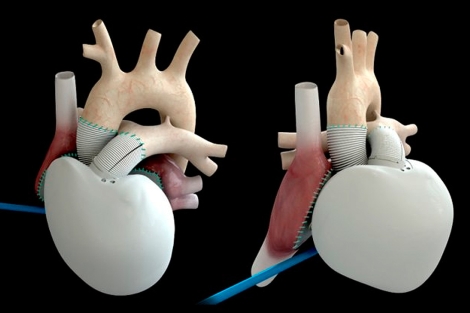
The ability to create these structures combined with the manipulation of stem cells could lead in the future to the creation of artificial organs. At least, scientist are working in this direction. A biological mold would be the basis to provide a three-dimensional structure to the organ. The outer casing would be scattered on cells which would colonize the structure resulting in specialized cells of the organ concerned (cardiomyocytes in the case of the heart, hepatomiocitos for the liver...).
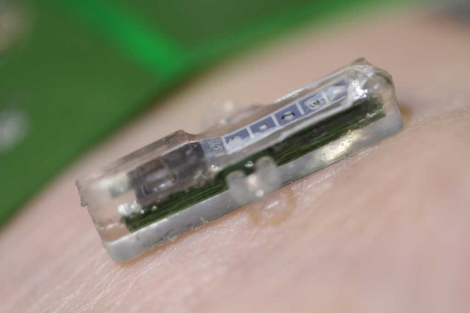
This possibility remains part of science fiction. What is beginning to be a reality is a new generation of 3D printers that generates human tissue. The company Organovo announced last April at the Experimental Biology Conference in Boston an equipment capable of producing tiny liver tissue samples (about 20 cell layers thick). This printer uses biological ink which in this case is made of three types of cells: hepatocytes, stellate cells and cells from the walls of blood vessels, obtained from waste coming from transplants and surgical interventions. Currently, the main use of these miniature livers is to test the effectiveness and impact of new drugs, but it may be the first step in a future technology able to print of organs for transplantation.
http://www.nejm.org/doi/full/10.1056/NEJMc1206319